 |
|
Periodontium:
Anatomy and Histology Review
THE GINGIVA
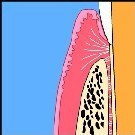
Composed of masticatory mucosa, it forms a collar around the tooth, 1-9mm wide, which is attached in part to the tooth and in part to the alveolar bone surface. With the exception of the palatal gingival, its apical border is the mucogingival junction which separates it from adjacent lining mucosa (Figs 1 and 2). On the palatal side, it blends with the masticatory mucosa of the palate.
DEFINITIONS
-
Gingival margin : The most coronal portion of the gingival.
-
Marginal gingival : That portion of the gingival just apical to the gingival margin.
-
Gingival sulcus : A shallow groove between the marginal gingival and the tooth surface, bound by sulcular epithelium laterally and juncitonal epithelium apically.
-
Gingival groove : Indentation along the oral or vestibular surface of the marginal gingival which parallels the gingival margin. It is located at about the same level as the apical border of the junctional epithelium. Note : its level does not correspond to that of the bottom of the sulcus.
-
Mucogingival junction : Demarcation line between masticatory mucosa of the gingival and the lining alveolar mucosa.
-
Interdental gingiva : The gingival which occupies the interdental spaces coronal to the alveolar crest. It is composed of a pyramidal interdental papilla in the incisor region. In the posterior region it is composed of an oral and a vestibular papilla joined by an interdental col. The interdental gingival, like the oral and vestibular portions of the gingival, is attached to the tooth by junctional epithelium coronally and by connective tissue fibers apically.
-
Free gingiva : Now discarded terminology. Formerly referred to that portion of the healthy gingiva believed to be "free," that is, not attached to the tooth. It included gingival tissue coronal to the connective tissue fiber insertion. Because junctional epithelium also attaches the gingiva to the tooth, this gingiva is no longer considered to be "free."
- Attached gingiva : Formerly referred to that portion of the gingiva attached to the tooth or alveolar bone by means of a connective tissue fiber insertion.
MICROSCOPIC FEATURES
- GINGIVAL EPITHELIUM (divided into 3 types)
Oral epithelium (OE): Stratified, squamous keratinizing epithelium which lines the oral (as contrasted to the dental) surface of the gingiva. It extends from the mucogingival junction to the gingival margin (except for the palatal surface where it blends with palatal epithelium).
Sulcular epithelium (SE) : Stratified, squamous epithelium, generally non-keratinized, which is continuous with the oral epithelium, lines the peripheral surface of the sulcus, and overlaps the coronal border of the junctional epithelium.
Junctional epithelium (JE) : Stratified non-keratinizing epithelium, in the shape of a collar with a cross-section resembling a thin wedge, attached by one broad surface to the tooth and by the other broad surface to the gingival connective tissue. New cells originate from apical cells and cells in contact with connective tissue. The desquamative surface is a t the coronal end which forms the bottom of the sulcus.
Unique features
-
The cells are largely undifferentiated and lack tonofibrils.
-
Intercellular junctions are less frequent that in OE or SE (junction density in JE is approximately 25% that of OE or SE).
-
The epithelium has 2 basal laminas, one which faces the tooth and one which faces the connective tissue.
-
Epithelial attachments : refers to the basal lamina and hemidesmosomes that connect the JE to the tooth surface.
-
The JE is more permeable than OE or SE to cells and fluids. It serves as the preferential route for the passage of fluid and cells from the connective tissue into the sulcus, and for bacterial products originating in the sulcus into the connective tissue.
-
In the presence of inflammation, it is readily ruptured by mechanical forces.
-
- CONNECTIVE TISSUE
Gingival fibers : The majority are composed of collagen fibers, with minor contributions from elastic fibers and oxytalan fibers (the fiber). Elastic and oxytalan fibers are generally confined to perivascular regions, although oxytalan fibers may appear as thin fiber bundles within collagen-rich regions.
- Dentogingival
- Dentoperiosteal
- Alveologingival
- Circumferential
- Semicircular
- Transgingival
- Intergingival
- Transseptal
Classification and anatomic distribution of gingival fibers:
Ground substance : Occupies the space between cells, fibers and neurovascular elements. Major components are water, glycoproteins and proteoglycans. Allows diffusion of biological substances between various structural elements.
Cells:
- Fibroblasts: Synthesis and resorption
- Macrophages : Participate in host defense and repair
- Mast cells : Participate in early phase of inflammation
- Undifferentiated cells : source of new cells
- Leukocytes (neutrophils, lymphocytes, plasma cells, etc…) : Participate in host defense.
- Osteoblasts, cementoblasts, osteoclasts, cementoclasts (will be described under “Periodontal ligament”).
Vessels and nerves :
- Blood supply : Capillary network subjacent to oral epithelium and junctional vessels originating from periosteal surface of alveolar bone, marrow spaces of alveolar bone and periodontal ligament.
- Lymphatics : drain principally to submaxillary lymph nodes
- Nerves : Braches of the traigeminal nerve provide sensory and proprioceptive functions. Autonomic nerve endings associated with vasculature.
Connective tissue-epithelial interatiions :
- May have a significant effect on tissue differentiation
DEVELOPMENT OF DENTOGINGIVAL JUNCTION
- Formation of reduced enamel (REE) epithelium composed of:
- Reduced ameloblasts which cannot divide
- Stratum intermedium cells which can divide
- Stellate reticulum cells which can divide
- Outer enamel epithelium which can divide
- Tooth eruption accompanied by:
- Fusion of REE with oral epithelium
- Progressive proliferation of outer layers of REE beginning at coronal end and progressing apically.
- Cellular proliferation of outer layers of REE gives rise to juncitonal epithelium (with a rapid turnover rate) which gradually replaces REE. In the process 1oepitheial attachment (REE to enamel) is replaced by 2o epithelial attachment (JE to tooth surface).
- Formation of dental cuticle
Stages in tooth eruption :
- Sulcus and junctional epithelium on enamel
- Sulcus on enamel, JE partly on cementum
- Sulcus at cemento-enamel junction and JE on cementum
- Sulcus and JE apical to CEJ.
CLINICAL CONSIDERATIONS
Periodontal probing : Does not accurately estimate sulcus or pocket depth. Probing depth generally overestimates anatomic sulcus or pocket depth because the probe actually penetrates inflamed tissues. The greater the inflammation, the greater the extend of probe penetration. Reduction of inflammation through periodontal treatment may reduce probing depth without necessarily producing new attachment of the periodontal tissues to the tooth.
Gingival margins of restorations in young people are more likely to become exposed as a result of passive eruption (apical migration of gingival margin causing increased exposure of the clinical crown).
Gingival tissue band forms a more stable interface with the gingival margin of a restoration than alveolar mucosa. If gingival tissue is absent, gingival grafts may be used to create new gingiva.
Gingival health is maintained primarily by control of microbial accumulations on teeth. The massaging effect of tooth cleaning procedures on tissue health is minimal.
Overhanging fillings contribute to periodontal disease primarily by favoring bacterial accumulation, rather than by direct irritation of the tissues.