 |
|
Periodontium:
Anatomy and Histology Review
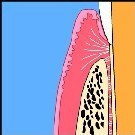
THE PERIODONTAL LIGAMENT
Fibrous connective tissue structure, with neural and vascular components, which joins the cementum to the alveolar bone.
FUNCTIONS
- Formative (fibroblasts, cementoblasts, osteoblasts)
- Resorptive (fibroblasts, osteoclasts, cementoclasts)
- Supportive (fibrous elements)
- Nutritive (vascular components and ground substance)
- Sensory (neural components)
ORIGIN
- Connective tissue of the dental follicle.
DEVELOPMENT
- Maturation begins at CEJ and proceeds apically
- Fiber bundles are reoriented perpendicularly to tooth and alveolar bone surface forming early Sharpey’s fibers in bone and cementum.
- Remodelling of fibers proceeds from mineralized surfaces toward central part of the ligament which is last to be remodeled.
- Sharpey’s fibers are mineralized fiber bundles which become part of the mineralized tissue matrix in which they are located (either bone or cementum). Although fiber bundles may be in part non-mineralized and located in the ligament proper, which the other part is mineralized as a result of becoming embedded in bone or cementum, only the part that is actually mineralized should be referred to as Sharpey’s fiber.
- Incompletely remodeled ligament or sections through neurovascular channels have been erroneously described as a so-called "intermediate plexus," a zone believed to allow for "slippage" between cemental and osseous fibers during rapid eruption. Such movement is more likely the result of continuous remodeling of the structural elements of the ligament.
D. PRINCIPAL FIBERS
- Primarily composed of collagen fibrils
- Alveolar crest f.
- Horizontal f.
- Oblique f.
- Apical f.
- Interradicular f.
- The periodontal ligament is composed of collagen fibres that originate as fibers of different diameters at the mineralized surfaces where the fibers are continuous with their mineralized portion (Sharpey’s fibers). These fibers are of a wider diameter on the bone side than the cementum side. They become unraveled into smaller fibers which join up with those of adjacent fibers to produce a meshwork of interconnected fibers oriented between bone and cementum. Fibres do not stretch cable-like from cementum to bone.
- Oxygen fibers : Generally run parallel to the root surface, although they can occasionally insert into cementum.
CELLS
- Fibroblasts
- Cementoblasts
- Osteoblasts
- Cell rests of malassez
- Vascular and neural elements
- Macrophages
- Cementoclasts
- Osteoclasts
- Undifferentiated cells
Neural elements tend to be myelinated near apical end and unmyelinated more coronally. Terminate as free or specialized endings within the periodontal ligament. Follow the distribution of the arterial blood supply.
CLINICAL CONSIDERATIONS
Thickness varies from 0.1 to 0.4mm with a mean around 0.2mm. Ligament is thicker in functioning than in non-functioning teeth, and in areas of tension than in areas of compression
Ligament cells are capable of remodeling ligament and adjacent bone when functional forces are altered or ligament is damaged.
Excessive forces can cause localized necorsis (cell death) that results in stoppage of remodeling at the affected site. Repair via cells from adjoining sites may be accompanied by localized resorption and ankylosis.
Accidentally exfoliated teeth can be replanted. Complications include external root resorption and ankylosis. These can be minimized by avoiding excessive handling of the torn ligament prior to replantation.
Appropriate therapy can halt progressive destruction of the periodontal ligament by periodontal disease and can result in partial repair of periodontal defects.