|

|
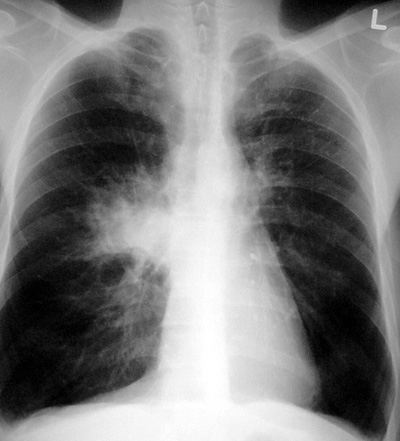
Small Cell Lung Cancer
Pathophysiology: A primary lung cancer derived from APUD cells. Often called oat cell cancer. The cancer has a marked
tendency to start centrally and invade the hila, mediastinum,
pericardium, and even the central bronchi and pulmonary
vasculature.
Usually seen with regional adenopathy and difficult to determine
how much of the mass is tumor and how much is nodal invasion.
Because of the primitive APUD origin, it is the commonest
lung cancer to be associated with the Paraneoplastic
Syndrome.
Clinical Clues: background of smoking.
Used to have terrible prognosis (6 months); much better now with
cysplatinum or analogues (maybe 5-6 years).
CXR/CT Findings:
-
Central lung nodule
or mass (3-6 cm) in upper 2/3 of lungs
-
Usually ipsilateral
hilar and mediastinal adenopathy
-
Mediastinal tumor
involvement (CT)
-
Encroachment of
central pulmonary vessels (CT)
-
Involvement of
central bronchi with post-obstructive changes:
atelectasis and/or pneumonia
Radiologic Clues:
-
In smokers of
cancer age group, any central mass must be considered to be
cancer.
-
In smokers of
cancer age group with any central pneumonia especially with
atelectasis, must rule out underlying central cancer.
FOLLOW all these patients with imaging to ensure
resolution.
-
Statistically,
primary lung cancer is in upper lungs; metastatic lung cancer
in lower lungs.
“Aunt Sophies”: gamut of central lung mass
-
Any primary central
lung cancer
-
Lymphoma
-
Metastatic cancer
with hilar/mediastinal nodes
-
Ipsilateral hilar
adenopathy: rarely sarcoidosis, silicosis, Castleman’s disease
-
Pulmonary
amyloidosis and nodal masses, rarely
-
Enlarged pulmonary
artery: acute embolism, tumor, marked dilation or aneurysm;
rarely
-
Silicosis,
berylliosis with dominant hilum
-
Drugs causing
adenopathy: (eg. dilantin, methotrexate, cyclosporine); rarely
|