|

|
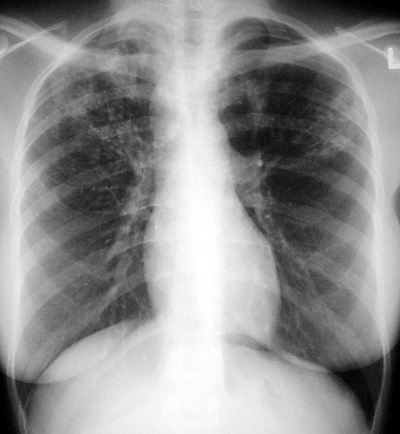
Tuberculosis - Primary
Pathophysiology: Tuberculosis (tuberculosis hominis)
is a CAP spread most commonly by droplet inhalation. The
infection is biphasic: a non-immune response (normal,
non-sensitive host) pneumonia occurs in the most ventilated
parts of the lungs ie. lower 2/3, followed in a few weeks with
tubercle bacteria draining into regional lymph nodes, regional
adenitis, tubercles entering the bloodstream with seeding
throughout the body particularly the reticulo-endothelial
system, and finally in about six weeks, the development of
immunity or hypersensitivity to tuberculoprotein (i.e. host is
now tuberculin positive).
With hypersensitivity, the normal host usually kills the
tubercle bacteria or renders them essentially inactive
(dormant). The pneumonia and subsequent clinical picture
resolve.
With overwhelming loads of bacteria, or in a normal
but genetically susceptible host, or in an
immunocompromised host, the disease may go unchecked. This
may lead to pleural effusions, miliary dissemination throughout
the lungs (miliary TB), or progressive primary tuberculous
pneumonia.
Clinical and Radiologic Clue: The commonest reason by far
in missing the early diagnosis of tuberculosis is that the
physician does not think about it!
Think tuberculosis! Tuberculosis is one of the “syphilis’
of the chest” and may look or mimic many disease
processes.
CXR/CT Findings: Primary TB
-
Focal area of
non-specific airspace pneumonia in mid or lower lungs
(non-specific) **
-
Regional
lymphadenopathy (much more specific) **
-
Pleural effusion
(so called ‘idiopathic pleural effusion’ when you miss
the diagnosis)
-
Miliary
tuberculosis: small micronodular millet seed-like lung pattern
-
Progressive
pneumonia with cavitation, fibrosis, architectural distortion
-
Rare: tuberculous
osteomyelitis of thoracic cage
-
Rare: empyema necessitates
-
Rare: tracheal,
bronchial regional tuberculosis
-
CT - “tree and
budding” sign: Non-specific but typical of the small
airways involvement of tuberculosis. Small bud-like
projections of peripheral interlobular bronchioles.
“Aunt Sophies”: Primary TB can be non-specific at onset:
- Any mid to lower lung focal pneumonia
- Causes of hilar or para tracheal adenopathy: eg. tumor, metastases, lymphoma
- Causes of pleural effusions: other para pneumonic effusions
- Miliary pattern: need to rule out TB. Other causes: small metastases (eg. thyroid), other infections (eg. mycoplasma), sarcoidosis
|